Cancer Stem Cells
Introduction/Background
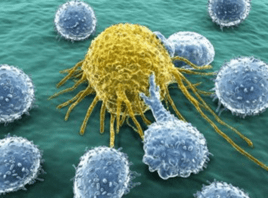
The cancer stem cells (CSCs) hypothesis was first proposed by Mackillop in 1983. He believed that cancers are heterogeneous tumors containing cells with various stem cell properties, the definition of CSCs given by AACR13 (American Association for Cancer Research) in 2006 is: cells in tumors that have the ability to self-renew and can produce heterogeneous tumor cells.
Cancer stem-like cells are a subpopulation of tumor cells that can drive tumor initiation and can cause relapses. Human cancer stem cells play an important role in tumor survival, proliferation, metastasis and recurrence: Essentially, cancer stem cells maintain the vitality of tumor cell populations through self-renewal and immortal proliferation; the movement and migration capabilities of cancer stem cells make tumor cell metastasis possible; cancer stem cells can stay in a dormant state for a long time and have a variety of resistance. Drug molecules are not sensitive to external physical and chemical factors that kill tumor cells. Therefore, tumors often recur for a period of time after most common tumor cells are eliminated by conventional tumor treatment methods.
Biomarkers of cancer stem cells are incompatible in cancers of different origins. In solid cancers, the clinical use of cancer stem cells specific biomarkers is limited, such as the carcinoembryonic antigen (CAE), fragments of the cytokeratin 19 (YFRA 21-1) and the alpha-fetoprotein (AFP). In addition, CD44, CD133, EpCAM, Sox2 and Nanog are also used in clinical. And in hematological cancer, CD44, CD123, CD33, CLL-1 and TIM-3 are the most relevant markers.[1]
Cell Culture Protocol
Take breast cancer stem cell culture as an example [5].
Breast cancer stem cells (BCSCs) culture mostly refers to the in vitro suspension culture system of human mammary epithelial stem cells established by MaxWicha.
Mammary epithelial stem cells grow in a suspension and undifferentiated form in a serum-free medium, which we call mammary stem cell spheres. In the primary culture, the cells were cultured at a density of 1000 cells/mL when subcultured on an ultra-low adhesion plate at 20000 cells/mL viable cells. Serum-free medium select serum-free mammary epithelial growth medium MEGM, supplemented with B27, 20ng/ml EGF, 20ng/mL bFGF and 4μg/mL heparin, without adding bovine pituitary extract. The mammary stem cell pellets were cultured for 7-10 days and then digested with 0.05% pancreatin and 0.53 mM MEDTA-4Na for 10 minutes, and the cells were collected in a centrifuge tube and centrifuged at 800 rpm. The cells obtained after centrifugation need to pass through a 40μm filter and observe whether they are single cells under a microscope. The number of clusters of two connected, three connected, and multiple cells in a 10,000 single-cell suspension should be between 30 and 150. If the cell cluster is greater than 100, the digestion and filtration steps must be repeated [5].
The Latest Research/Application
Targeting CSC has been the focus of cancer research for many years.
CSC targeted therapy methods include kinase inhibitors and targeted stem cell related pathways, such as β-catenin and Wnt, some of which have entered the clinical stage. CAR T-cellular therapy has showed exhilarative clinical efficacy in the treatment of hematological diseases. Recently two CAR-T cell based therapeutics, Kymriah (Tisagenlecleucel) and Yescarta (Axicabtagene ciloleucel) are now used for treatment of B cell acute lymphoblastic leukemia and diffuse large B-cell lymphoma respectively in the US.[1]
Based on the gratifying results of CAR T-cellular therapy in the treatment of hematological diseases, CAR-T cell-based methods have also entered the treatment of solid cancer. In this regard, most research focuses on improving CAR-T cells and overcoming the adverse effects of tumor microenvironment on solid tumors.[2] For example, research on CAR-T cell therapy for different TAAs in Triple-negative breast cancer (TNBC) has steadily increased, directly redirecting the patient’s immune system to identify and eradicate tumor-associated antigens (TAAs) expressing tumor cells as a treatment for TNBC. [3,4]
Conclusion/Future Perspective

Therapies for cancer stem cells are a hot spot in the field of tumor treatment and prevention of tumor metastasis, which help to save the patients and clinics from high personnel, emotional, and medicinal costs, significantly improving the outcomes for patients. It is worth noting that improvement of target specificity and decreased off-target effects are specially needed. In the treatment of solid tumors, its efficacy and safety also need to be improved.
Where to Get Cancer Stem Cells?
AcceGen provides various types of Cancer Stem Cells, such as Human Breast Cancer Stem Cell, Human Colon Cancer Stem Cell, Human Glioma Cancer Stem Cell etc. More other types of leukemia cell lines are available in AcceGen: Cancer Stem Cells.
AcceGen cancer stem cells have good self-renewal and differentiation capabilities.
It is our pleasure to help relative researches to move forward. All the products of AcceGen are strictly comply with international standards. For more detailed information, please visit our product portfolio or contact inquiry@accegen.com.
Reference
[1] https://www.frontiersin.org/articles/10.3389/fimmu.2020.01280/full
[2] https://pubmed.ncbi.nlm.nih.gov/31754328/
[3] https://pubmed.ncbi.nlm.nih.gov/32795486/
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586061/
[5] https://pubmed.ncbi.nlm.nih.gov/26040679/
Comments
Post a Comment